iPSC derived retinal organoids: A promising tool for modelling retinitis pigmentosa
Retinitis pigmentosa (RP) is a group of degenerative disorders of the retina, caused by mutations in one of more than 60 genes, including the genes for making rhodopsin, pre-mRNA processing factors and usherin. The genes associated with RP play essential roles in the structure and function of photoreceptors and their supporting cells, retinal pigment epithelium, hence, mutations in these genes cause progressive degeneration of both rods and cones.
RP is one of the most common inherited forms of sight loss, affecting more than 1 million people worldwide. The genetic disorder has multiple modes of inheritance, including autosomal dominant, autosomal recessive, X-linked, dihybrid inheritance and mitochondrial genetic.
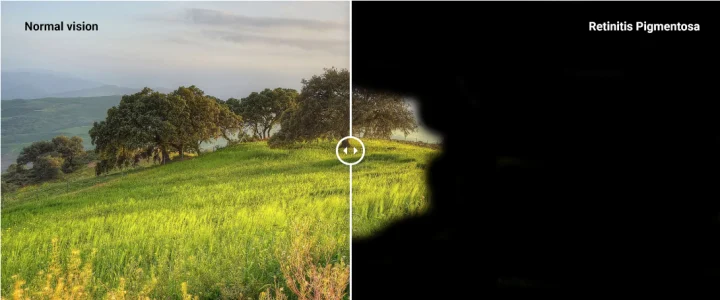
An initial clinical feature of the disease is night blindness, since rod photoreceptors, which are responsible for vision in low light, degenerate before cones. Other symptoms that typically follow include visual field constriction, loss of central vision and defects in colour vision, due to the degeneration of cone photoreceptors. Currently, there are no effective treatments for RP and so visual prognosis is poor.
Living with the disease can be extremely challenging. Merroney, aged 41, whose mother also suffers from RP, was diagnosed with autosomal dominant RP1 at the age of 23. She currently has around 30% visual field in both eyes and explains that the effects of RP can be terrifying, particularly in the dark. Merroney says that social situations with people she’s never met before can be awkward: “Because I often don’t see that the person has gone to shake my hand for example, I worry I come across as rude”. Due to night blindness, she worries about picking her children up from school in the winter.
We asked Merroney whether the disease affected her decision to have children. She explained that there is a level of guilt surrounding the prospect of passing on the gene but remains positive in the hope that in her children’s lifetime, considerable advances will have been made in the research of treatment for RP.
Ongoing RP research focusses on gene and stem cell therapy and the value of antioxidants, amongst other treatment strategies. Studies by the University of Iowa and Columbia University have demonstrated that patient skin-derived induced pluripotent stem cells (iPSCs) harbouring a pathogenic gene mutation, can have the mutation corrected using CRISPR/Cas9 gene editing technique.1 Additionally, researchers from the University of Pisa, Italy have presented data demonstrating the benefits of a diet rich in antioxidants in preventing progression of the disease in animals.2 Currently, there are over 200 clinical trials 3 in progress studying the potential of new and existing therapies to cure or alleviate the symptoms of this devastating disease, and over 60 companies have programmes focused in the field.
Present understanding surrounding RP has relied mostly on animal models, which are not always representative of the human system. Rodents, which are commonly used as a model, have limited use driven by differences in some key features, including lack of a cone rich area called macula, reliance on scotopic (night) vision and poor recapitulation of human disease phenotype. IPSCs provide an opportunity for establishment of model systems relevant to human physiology, with more complex tissues such as retinal organoids allowing the study cell-cell interactions and responses to light as a measure of function. They also provide an excellent platform for disease modelling, as well as for drug development and toxicity assays.
In collaboration with Newcastle University, Newcells Biotech has developed an in vitro platform using human iPSC–derived retinal organoids and retinal pigment epithelium cells that allowed investigation of disease mechanisms of RP, with the potential to be used in pre-clinical assessment of drug safety and efficacy 4. The iPSC-based retinal organoid and retinal pigment epithelium assays can model either healthy or diseased retina and overcome a number of the limitations of existing models, allowing for target engagement and drug efficacy studies for retinal diseases, such as RP.
References
- Bassuk, A.G., Zheng, A., Li, Y., Tsang, SH., Mahajan, V.B. Precision Medicine: Genetic Repair of Retinitis Pigmentosa in Patient-Derived Stem Cells. Scientific Reports. 2016; 6: 19969. Available from: doi: 10.1038/srep19969
- Piano, I., D’Antongiovanni, V., Testai, L., Calderone, V., Gargini, C. A Nutraceutical Strategy to Slowing Down the Progression of Cone Death in an Animal Model of Retinitis Pigmentosa. Frontiers in Neuroscience. 2019; 13:461. Available from: doi: 10.3389/fnins.2019.00461
- Biopharma Insight Clinical Trials database, accessed online, June 2019
- Buskin, A., Zhu, L., Chichagova, V., Basu, B., Mozaffari-Jovin, S. et al. Disrupted alternative splicing for genes implicated in splicing and ciliogenesis causes PRPF31 retinitis pigmentosa. Nature Communications. 2018; 9:4234
Share on social media:
Don't miss out on our latest innovations: follow us on Linkedin